
Elena Gómez Díaz, Instituto de Parasitología y Biomedicina López-Neyra (IPBLN-CSIC)
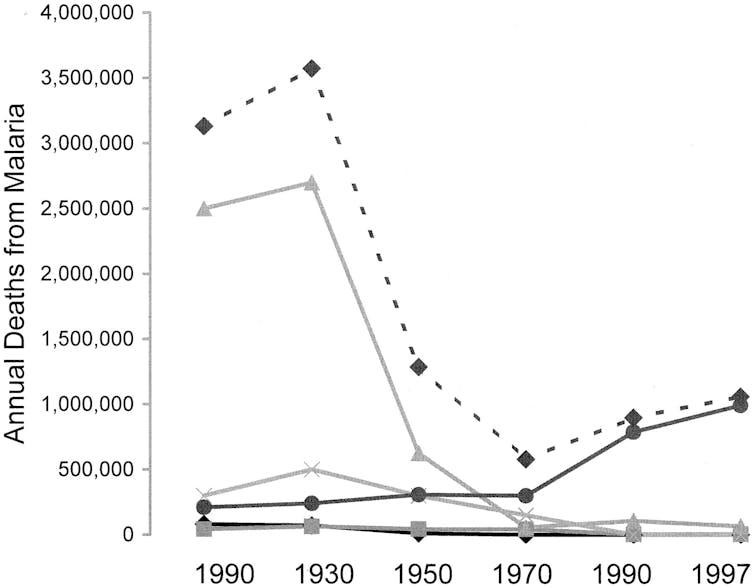
Malaria has been a terrible disease throughout human history. Deaths actually peaked over five million in the 1930s and it spread all over the world. Following a first global eradication programme launched by the World Health Organization (WHO) with massive spraying campaigns using the dichlorodiphenyltrichloroethane (DDT) insecticide, Europe was declared malaria free in 1975.
Today, we face a very different scenario. There has been a major reduction in the malaria burden, from millions to about half a million deaths a year in 2018. Even so, malaria is still one of the three leading causes of death in developing countries. And it’s estimated that 40% of the world’s population (more than 200,000) is at risk. In addition, two thirds of malaria deaths are children under the age of five.
Africa is home to 70% of the world’s malaria cases and 90% of deaths. What we’ve learnt from Africa is that malaria and poverty are intimately connected. The lack of basic sanitary services and hygiene, limited access to drinking water and electricity, and poor economic resources, limit drug and vaccine administration campaigns and mosquito control interventions.
We should think about something as simple as the logistics required for delivering a vaccine that must be kept at 4 ⁰C when the outside ambient temperature is 40 ⁰C. Or buy antimalarial medications and mosquito nets when your income is less than one euro a day.
The second major problem is education. Illiteracy rates in Africa are very high and religious and cultural beliefs about diseases and death are deeply rooted. The overall knowledge of malaria prevention practices among a large portion of women in both urban and rural settings is generally low. Therefore, the effectiveness of new anti-malaria strategies is strongly compromised if local communities aren’t educated about prevention and treatment.
Finally, the third reason’s name is Plasmodium falciparum. This species is mainly in Africa and is responsible for 90% of global malaria deaths. Malaria infection caused by this particular species, without early diagnosis and treatment, often leads to death.
So in the age-old battle against malaria, what are researchers doing to fight the disease?
A powerful enemy
Drug discovery and vaccine development are at the forefront of malaria research and innovation. Still scientists seem to be losing the dangerous race to eliminate the deadly malaria parasite.
The most hopeful strategy in recent years has been the use of the so-called “Transmission-blocking vaccines” (TBVs). TBVs’ goal is to induce antibodies in humans, which are then taken up by mosquitoes together with the parasites during a blood meal. These antibodies then interfere with the sexual development of the malaria parasite inside the mosquito, blocking the transmission of the disease to a healthy person.
Advances are slow. The reality is that till today there is still no highly effective licensed malaria vaccine. And Plasmodium falciparum has developed resistance to all antimalarial drugs such as chloroquine and artemisinin derivatives.
One of the main challenges facing malaria elimination, is the incredible capacity of the malaria parasite to adapt to a changing environment. When it comes to cope with environmental change, the malaria parasite is a master of stealth.

Master of stealth
An organism can display different phenotypes when exposed to different environmental conditions. This plasticity is related to epigenetic mechanisms. Epigenetics is the study of chemical modifications that activate and deactivate parts of the genome, inducing changes in the expression of genes, that are independent and not caused by changes in the DNA sequence.
Epigenetic processes are key in the adaptation potential of the malaria parasite in response to signals from the environment. These mechanisms are the basis, for example, of immune evasion strategies that allow the parasite to vary antigenic proteins at the surface of infected red blood cells and this way hijack our immune defences. How this variability and plasticity is achieved, is an important question in the field that remains unresolved.
One reason is that malaria studies, to date, have focused on the blood stages of the parasite during the life-cycle in humans. But we know very little about the biology of the parasite during its life cycle in the mosquito. This is in spite of that fact that inside the insect host is where the sexual reproduction that creates new variability occurs.

Another serious problem for malaria research is the enormous diversity of parasites and the natural variability that exists in endemic areas. This means that doing research in the field in Africa is essential.
To fill this gap in our knowledge, our research focuses on the malaria life cycle in the mosquito and uses parasites isolated from areas of endemic malaria transmission. We aim to discover which are the epigenetic mechanisms underlying the formidable adaptation potential of the malaria parasite. And, with that, try to find its Achilles heel.

Our research in Africa
Since 2013 we have been conducting research in the south of Burkina-Faso in collaboration with the country’s “Institut de Recherche en Sciences de la Santé”.
This is an area of high malaria transmission, where 100% of the population is at risk, and where a lot of families live in poverty. Around 30% of the population lives on less than one dollar a day. In 2018, there were an estimated 8 million cases of malaria (in a population of 14 million people) and 28,000 deaths, according to the WHO.
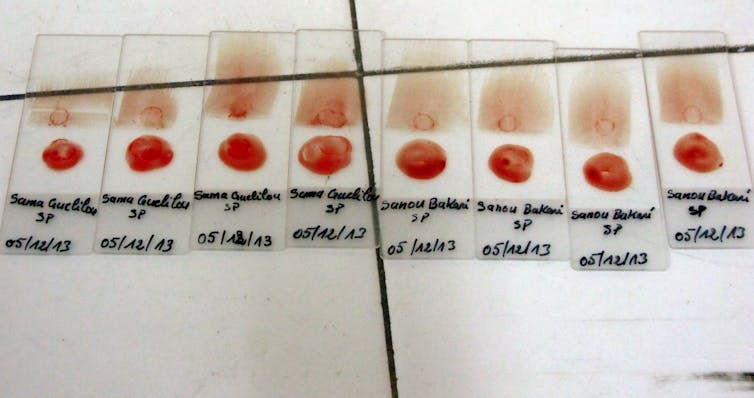
Our projects contribute to the diagnosis and treatment of malaria. But working in Africa implies high risk and uncertainty. It can be a logistical nightmare, due to the lack of appropriate scientific equipment and infrastructure. And it can also be dangerous, because of the health risk associated to multiple infectious diseases as well as the political instability.
Aside from the science, our research has a development and international cooperation facet by providing economic resources to the region. This is scarce because of the insufficient scientific funding in Spain. Nevertheless it contributes to covering the cost of the antimalarial treatment and to hiring technicians.
Our investigations also benefit the transfer of knowledge between researchers from Europe and in Africa. This is done mainly, through the scientific training of Burkinabe students and young researchers that face enormous challenges and difficulties to develop their research careers in their countries of origin.
Moreover, these field campaigns take place in coordination with local schools and health centres. They also serve to communicate with the community about what scientists do and why they engage with them in research activities, to drive change.
Elena Gómez Díaz, Investigadora Ramon y Cajal. Líder de un grupo de investigación de epigenómica en malaria, Instituto de Parasitología y Biomedicina López-Neyra (IPBLN-CSIC)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
