
Edward Parker, London School of Hygiene & Tropical Medicine and Beate Kampmann, London School of Hygiene & Tropical Medicine
For many of us, the threat of coronavirus suddenly feels much closer to home. The last few days have seen a rapid increase in the number of cases in South Korea, Iran and Italy. Now officially a pandemic, the virus has proven adept at crossing borders, with confirmed cases reported in over 100 countries (for the latest numbers, refer to our coronavirus mapping tool).
In the face of this escalating outbreak, it can be difficult to gauge how concerned we should be. What threat does the coronavirus pose to us as individuals? And what are the broader societal risks of this outbreak? Answering these key questions can help place the daily headlines in context.
Individual risks
Fear for our personal safety is an understandable instinct when faced with minute-by-minute coronavirus updates. Fortunately, our understanding of the clinical effects of this novel virus is improving with each passing day.
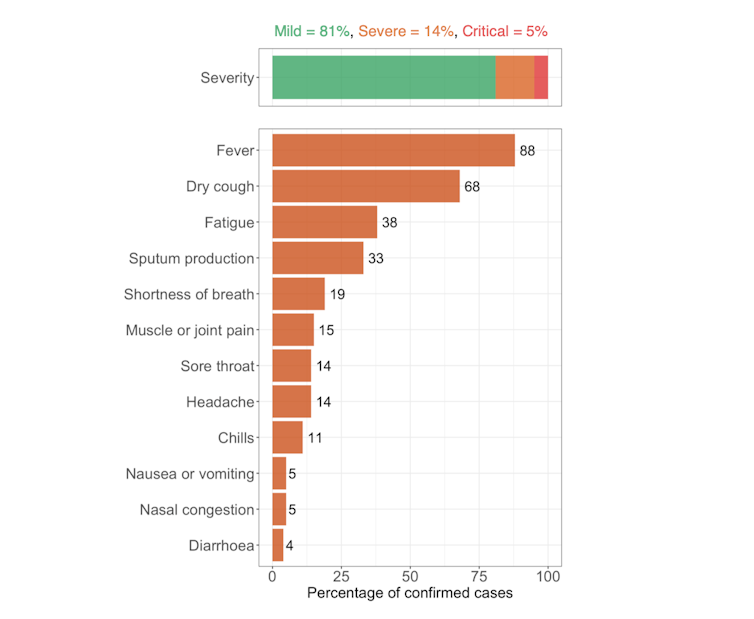
Based on data from over 44,000 confirmed cases in China, we know that roughly 80% of people have mild illness, 14% have severe disease (for instance, involving shortness of breath or reduced blood oxygen levels), and 5% become critically ill (suffering respiratory failure, septic shock and/or organ failure). If many mild cases are going undetected, the proportion of severe and critical infections may turn out to be lower once the dust has settled.
The proportion of reported cases of a disease that lead to death is called the case fatality rate (CFR). Estimating the CFR for the coronavirus disease (COVID-19) is challenging when uncertainty over the total number of infections remains. As things stand, our best estimates put this value in the range of 0.3% to 1%. This is lower than the 10% CFR of the Sars outbreak that affected China in 2003, but up to ten times higher than the less-than-0.1% CFR of a typical flu season.
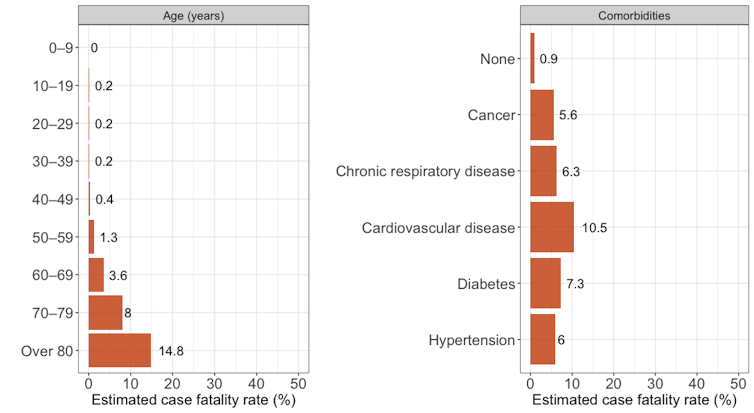
However, it is crucial to remember that the CFR is not a fixed entity. It varies according to age, health condition and the level of clinical care available to people who become severely ill. Among confirmed cases in China, the estimated CFR is less than 0.5% in under-50s but rises to almost 15% among over-80s. The fatality rate is also substantially higher in people with other conditions, such as cardiovascular disease (10.5%), diabetes (7.3%) and chronic respiratory disease (6.3%).
The message is clear – reducing the risk of exposing high-risk people is key to our individual and societal response to the coronavirus outbreak. Or to put it bluntly, don’t visit elderly friends or relatives if you feel at all unwell.
Many uncertainties remain. For example, under-20s made up less than 3% of the confirmed cases in China and no deaths were recorded in children under ten. This is comforting news, but raises questions over whether school closures – a key strategy used to combat the 2009 swine flu pandemic – will help slow down the spread of coronavirus.
Early reports suggest that pregnant women are not at greater risk of severe illness with COVID-19, in contrast to both Sars and influenza. There is also currently no evidence of transmission to babies in the womb or via breastmilk. But continued monitoring of how the virus affects pregnant women will be crucial as cases of this new disease rise.
Societal risks
The fact that most cases of COVID-19 are mild may seem at odds with the alarming coverage of the outbreak. While panic is neither helpful nor warranted, we must also guard against complacency.
As the virus spreads through susceptible populations, the numbers quickly add up. Recent reports from Italy suggest that around 10% of confirmed cases require admission to intensive care units. As the epidemic ignites in more and more countries, COVID-19 is poised to place a huge strain on health systems across the globe. In the northern hemisphere, this surge arrives at a time when hospitals are already racing to keep up with the demands of winter.
As a result, social distancing measures (such as self-isolation, workplace closures and the cancellation of public events) are likely to play an important role in the evolution of the pandemic. The torrent might not be prevented, but slowing it down is our best chance of ensuring the dam will hold.
The stakes go beyond coronavirus. During the 2014 outbreak of Ebola in West Africa, deaths from malaria, HIV and several other causes rose dramatically as health systems buckled under the pressure of the unfolding epidemic. The more resources that COVID-19 absorbs, the larger the ripple effects throughout our health systems will be.
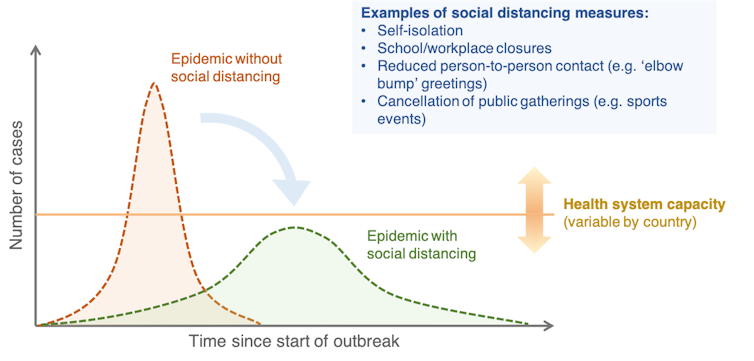
Fortunately, we know that quarantine and containment can be effective against COVID-19. According to a recent WHO report, the stringent measures enforced in China have “averted or at least delayed hundreds of thousands of COVID-19 cases in the country”. It is likely that the measures brought in across Italy this week will have a similar effect in curbing the course of the outbreak.
What is far less certain is whether measures short of a total lockdown can keep the virus at bay. Early self-isolation, frequent handwashing and voluntary social distancing are being promoted in many countries, and the economic and social incentives for avoiding more drastic measures are substantial. But if the number of cases continues to rise, we must prepare for the possibility that more stringent measures will be needed.
Individual acts matter
Most of us will stay healthy throughout the coronavirus outbreak, and we must therefore quell our instinct for panic. But we all have a social responsibility to help keep this pandemic under control. We can do this by knowing how to recognise the symptoms of COVID-19, by staying up to date on local guidelines on what to do if we exhibit them, and by taking stringent social distancing measures. Every act that slows down the spread of the virus can make a difference.
Protecting the vulnerable in our communities should now be imperative to us all. At a time of social distancing, our social conscience will determine the fallout from this public health emergency.
Edward Parker, Research Fellow in Systems Biology, London School of Hygiene & Tropical Medicine and Beate Kampmann, Director of The Vaccine Centre, London School of Hygiene & Tropical Medicine
This article is republished from The Conversation under a Creative Commons license. Read the original article.
